The information you are about to read was first written and researched for a lecture I gave. I received a lot of requests for notes or the outline to the lecture. I have provided a summary box at the bottom if you are not interested at how I arrived at the dietary guidelines, but just want to know what to eat and what not to eat.
As someone who also couldn’t believe the misinformation online, I hope this will provide evidence based truth for preventing and reversing cardiovascular disease.
What are the True Causes of Heart Disease and Stroke?
Coronary heart disease is a disease of the blood vessels supplying the heart muscle. Ischemic strokes are the result of a clot in the blood vessel, while hemorrhagic strokes are caused by a rupture of a blood vessel. So what we are really trying to understand when looking at the cause of heart disease and stroke:
1. What is causing damage to the blood vessels, making it constrict, causing clots, and making them vulnerable to damage like calcification (measured by you calcium score indicating calcium is going into the arteries instead of the bones), glycation (measured by your glycated hemoglobin known as HbA1C) and risk of oxidation (measured by the type of LDL, not the total number)
2. What is cholesterol’s role, and therefore Statin drugs in this process?
The Top Main Risk Factors for Inflammation, and therefore Heart Disease and Stroke include:
1. Obesity, high blood sugar, oxidized cholesterol, high blood pressure and non-alcoholic fatty liver disease from a diet high in sugar (esp. high fructose corn syrup), trans-fats (hydrogenated oils), refined vegetable oils (soy, corn, canola, sunflower and safflower), excessive amounts of refined grains (esp. wheat) and a lack of exercise.
The US has the highest obesity rate in the world, and studies have shown that people with a fasting blood sugar level of 100-125 mg/dl had a 2.5 fold increased risk of having coronary heart disease than people with a level below 79 mg/dl.
According to a study from the American Journal of Cardiovascular Disease, the consumption of oxysterols from commercially fried foods, oxidation of cholesterol driven by consumption of excess polyunsaturated fatty acids from vegetable oils, smoking, trans fatty acids from partially hydrogenated vegetable oil, and lifestyle factors likely underlie the persistent national burden of heart disease.
Up to 80 percent of strokes are preventable. According to researchers, lifestyle factors such as diet, exercise, body mass index, blood sugar levels, blood pressure, vitamin D status, stress, and smoking can have a direct bearing on your individual risk.
The rate of strokes among those younger than 55 nearly doubled between 1993 and 2005 – and this rise is likely due to increasing rates of risk factors like obesity, diabetes, and high blood pressure.
2. Smoking, medications, binge drinking and other toxic ingestion and exposure, especially when coupled with a deficiency in vitamin C.
3. Stress, Depression, and Diabetes. In a recent study, 86 percent of people were more likely to have a stroke or mini-stroke from depression, 59 percent more likely to have a stroke or mini-stroke from the highest chronic stress, and more than twice as likely to have a stroke or mini-stroke from hostility.
Interesting enough, anger wasn’t a risk factor. The World Health Organization is projecting that, by the year 2020, depression will become the world’s second most devastating illness, after heart disease.
Women are twice as likely to get depression than men, especially around the stressful time periods of childbirth and menopause. Estrogen increases the activity of the enzyme – endothelial nitric oxide synthase (eNOS) – that causes tissues to swell and blood vessels to widen, resulting in rashes, breathing issues and even cardiac arrest.
The balance of estrogen and progesterone are important, as normal nitric oxide production is healthy but too little or too much can be harmful.
Those with Type 2 diabetes are up to 4 times more likely to get heart disease, and 65% of those with diabetes die from heart disease or stroke.
4. Hypothyroidism and Hyperthyroidism. Many thyroid disorders are linked to a deficiency in iodine and selenium and toxicity from soy oil, fluoride, and chloride from unfiltered drinking water supplies, brominated vegetable oils from sodas and sports drinks, and bromides from pesticides and commercial bread.
5. A deficiency in vitamin K2 and magnesium that leads to calcification of the arteries, and a deficiency in CoQ10, vitamin C, E and carotenoids that weaken blood vessels and make cholesterol prone to oxidation.
The Highest Rates of Heart Disease and Stroke in the US Gives US a Clue

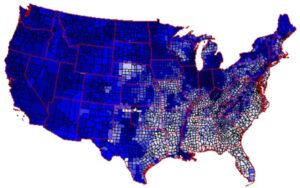

If you look at the US map of heart disease and stroke, you will see a major cluster of rates of heart disease and stroke highest in the southeastern US, and lowest in the west for both men and women.
The states in the South also have some of the highest rates of obesity, smoking, sugar, vegetable oil consumption, depression, sedentary lifestyle, hypertension, and diabetes; all the major risk factors for heart disease and stroke. What is VERY interesting, is the depression rates and the heart disease are coincidentally close to each other in many states. Is our diet making up depressed?
I recently discovered after writing an article titled Mental Health Starts in the Gut, Not the Brain, that the vitamins and minerals that are required in sufficient amounts for all of your neurotransmitters to work properly to prevent anxiety and depression, are the EXACT same ones that help prevent heart disease and strokes.
The third map is taken from the USGS, and shows where the soils are lacking magnesium. The lighter the color, the less magnesium is in the soil. As you can see, the southeast is the most deficient.
The Lowest Rates of Heart Disease around the World
While it is hard to pin down the latest statistics, here are five countries that have recorded the lowest rates of heart disease deaths:
1. Hong Kong
2. Japan
3. France
4. Spain
5. Greece
When looking at France, scientists are often dumbfounded because everything that mainstream US medical industry believes about dietary cholesterol, saturated fat and heart disease get turned on its head. It has been dubbed the “French Paradox.”
The French eat four times as much butter, 60 percent more cheese, more red meat, nearly three times as much pork and have a ten percent higher rate of smoking.
The French and the Swiss are considered the slimmest people in Europe, and the United States is ranked #1 for obesity in the world. Obesity (especially belly fat) from a diet high in sugar (mainly high fructose corn syrup), fried foods in vegetable oil (all fast food and the majority of restaurants) and refined carbohydrates leads to inflammation, high blood pressure, diabetes, inactivity and therefore blood vessel damage, heart disease, and stroke.
Saturated Fat and Heart Disease: Poor Evidence
In the past, the US focus on heart disease and stroke risk from a dietary standpoint has zeroed in on saturated fat and dietary cholesterol. In a recent January, 2010 meta analysis from the American Journal of Clinical Nutrition over 23 years, it showed no correlations of all saturated fat intake (like red meat, animal fat, eggs and dairy) to heart disease and stroke. Another meta-analysis from 2010 that looked over 20 studies, also found no correlation from red meat consumption to heart disease and diabetes.
What if it is actually the high intake of saturated fat and cholesterol that is protecting the French? Or is it vitamin K2 rich fat? A study from the Journal of Clinical Endocrinology & Metabolism reported that a low-fat, high-fiber diet (which has also been found to deplete heart-healthy vitamin D 43% faster) reduced testosterone levels in middle-aged men, with a diet containing less than 40 percent of energy as fat (including saturated) lead to a decrease in testosterone levels.
We also have to consider a cleaner agricultural system in France. When we look at a study from Brazil – who have also embraced genetically modified crops and therefore heavy pesticide and herbicide use – we find that these chemicals lower testosterone and increase estrogen.
Chemical agriculture was introduced in the early 1900’s, and use has been compounding since then along with our disease rates. GMO’s have pushed this amount even further despite promises that it would require less chemicals. Instead, nature created super weeds.
Men whose testosterone levels were slightly above average were 45% less likely to have high blood pressure, 72% less likely to have experienced a heart attack and 75% less likely to be obese than men whose levels were slightly below average. The optimal level appears to in the 550-900 ng/dl range to reduce risk according to the American College of Cardiology.
Animal Fat for Heart Health?
In the Gascony region, you will also find goose and duck fat are slathered on bread instead of butter, people snack on fried duck skin and eat twice as much foie gras as other Frenchman, and fifty times as much as Americans.
During a 10 year epidemiological study of food surveys by Dr. Serge Renaud, he concluded that the Gascons eat a diet higher in saturated fat than any other group of people in the industrialized world, and have the lowest rate of death from cardiovascular disease in all of France.
High-fat diets have been observed in several indigenous populations with the absence of heart disease. The Inuit who survive on almost entirely seal meat and fish, the Masai tribe in Africa that subsist only beef and raw milk, and the Pacific Islanders with their high consumption of coconut meat and oil (saturated fat), fish, tubers, and fruit.
In all of these, some have low cholesterol in the 140’s and 150’s like the Masai, and some have high cholesterol up to 250 like the Pacific Islanders. This shows a benchmark range that is free of heart disease if only looking at cholesterol numbers, and this tells us that there is much more to picture when assessing risk.
Does this Apply to Everyone?
Just like we have to be careful about making sweeping generalizations about saturated fat and cholesterol, we also need to be careful when extrapolating conclusions from certain populations and applying it to everyone.
All you have to do is look at the saturated fat intake difference between France and Japan, yet still, both are ranked in the top 5 for the lowest levels of cardiovascular disease.
As I have learned doing nutrigenomics analysis programs at Nutrition Genome, there is never a one size fits all system. When we start to look at individual genes and biochemistry, we see a difference in the type of fat and how it is broken down from person to person.
Some people will thrive on a higher fat diet, while others may experience more inflammation and even insulin resistance. So while the French or Inuit may thrive on fat, people with other heritage may thrive more on a lower-fat diet. This is why genetic testing is so invaluable.
Trans-Fats and Vegetable Oils: The True Cause of the Increase of Heart Disease and Strokes
The government has been telling Americans for the last 60 years or so that saturated fat and cholesterol is the cause of heart disease and to adopt a low-fat diet, so they can’t exactly admit they have been wrong all along (they are). The majority of fat consumed in the US has come in the form of hydrogenated oils or trans-fats and vegetable oils, especially soy oil in restaurants and processed food because it’s cheap.
In the U.S., we saw a period of heart disease skyrocketing from 1920-1960. Before that it was relatively unknown. From 1920-1980 we saw a percentage of dietary vegetable oils in the form of margarine and other hydrogenated oils, and refined vegetable oils increase about 400 percent while the consumption of sugar and processed foods increased about 60 percent.
Today, it is estimated we eat 100,000 times more vegetable oils than in the early 1900’s. It is the single biggest increase in any kind of food nutrient over the course of the 20th century. Check the back of most salad dressings, cookies, crackers, chips and bread and you will find vegetable oils. Almost every single restaurant in the US used hydrogenated oils – or trans-fats – to cook with and now use vegetable oils in their place since trans-fats were banned in 2007.
When vegetable oils are heated – say in fried, baked or sautéed food, they create more than 100 dangerous toxic oxidative compounds; the exact type that causes inflammation and arterial damage that leads to heart disease and strokes.
Dr. Fred Kummerow, who is now almost 100 was the first to publish a paper in 1957 pointing towards trans-fats as the cause of heart disease, not cholesterol. “Trans fat was put in the diet in 1910, and it was in the diet until 1965, when I was a member of the American Heart Association committee on fats. And when these fats were eaten by people, they didn’t develop any prostacyclin. Prostacyclin is a component in the blood that prevents the clotting of blood. So if you don’t have any prostacyclin, you can’t clot your blood. And a lot of those people ate a diet of sudden death.”
Dr. Kummerow eats a a whole egg every day. ““The egg contains all of the amino acids that you need. Now, amino acids are present in different foods, but most all of them are present in animal fat, like cheese, beef, pork, eggs, chicken, and fish. They are complete amino acids. So if you eat those kinds of foods, you will have all of the amino acids that you need to build what is called endothelin cells, and they carry all the functions in the body that cause life.”
The truth is that saturated fat and cholesterol (foods like eggs, meat, butter, coconut oil and liver) are actually some of the most nutrient dense foods available, with crucial b-vitamins and fat soluble vitamins A, D, E and K that make your heart healthy.
The prevailing dogma about saturated fat and cholesterol has been wrong both biochemically and clinically. If you look at breast milk – considered the perfect food for life – it has a higher amount of cholesterol than any other food on the planet. An estimated 50% of its calories are from fat, much of it saturated. And this is the percentage of fat when our hormones start working optimally. What does that tell us about our requirements for dietary cholesterol and saturated fat?
In the US, we do have to be more selective about the saturated fat.
In most of Europe, you will not find feedlot farms where animals are fed strictly grain. They are out in the pasture and the words “grass-fed” and “local” will generate a quizzical stare.
In the US, factory farmed animals are fattened up quickly on chemical laden soy and corn, creating high toxic loads in the fat and high omega-6’s (the same pro-inflammatory compounds in vegetable oils and are 19x higher in feedlot eggs). Grass-fed meat is 2-4x higher in omega-3 content, 4x higher in vitamin E and 500 percent higher in CLA, the compound known to be anti-carcinogenic, reduce abdominal fat, anti-diabetic and anti-sclerotic. Always look for “grass-fed” and “pastured.”
Alcohol and Heart Health: What is the Truth Regarding Wine?
When the French Paradox became popular, the US researchers concluded it must be the the resveratrol and quercetin in the wine that are making the French so healthy.
As I mentioned earlier, they are basically going to pretend they weren’t wrong about saturated fats and shift the focus. Within a year of this hypothesis, wine consumption went up 44% within a year in the US. But we didn’t get the same results as the French.
I believe this happened for a few reasons. First, because we kept our sugar, vegetable oil consumption and weight the same while not adopting the other habits of moderation that the country is known for. Small meals that are fresh from the farm, consumption of saturated fat and cholesterol balanced with plant foods, lots of walking and biking, small waistlines, and more leisure for stress relief.
Second, the wine in the United States is not the same as in France or other parts of Europe. When you break down the pesticides, fungicides, insecticides and multiple additives used for color, body and flavor allowed in US wines, it becomes no different than other processed foods. The majority of wines in Europe are still produced the way they have been for thousands of years, preserving the health benefits of unadulterated wine. There is a reason people consistently comment about how the bread and wine doesn’t bother them when they visit Europe.
The latest study on alcohol from Harvard was published this month in the European Heart Journal, and is perhaps one of the longest of its kind. It followed 14,629 men and women aged 45-64 and followed them for up to 25 years.
They found that for those who drank one 5 oz glass of wine or 12 oz. beer per day, the men had a 20 percent less incidence of heart disease and 16 percent for women. What’s interesting is that heart failure rates were higher for those who drank less OR more.
For those having more than 21 drinks, a higher risk of dying from any cause went up 47 percent for men and 89 percent for women. One way to read between the lines of this study, is that the people who were moderate with their alcohol intake at 5 oz. per day, were most likely moderate in their diet and exercise habits, and therefore body weight.
What we have seen in our nutrition practice is the daily consumption of 1-2 glasses of wine leads to excess body weight in the belly, sinus congestion and disrupted sleep, especially in women. This is because our other lifestyle habits are still in place, and therefore alcohol serves to compound the problem. But in an individual with healthy diet and exercise habits, and a healthy body weight, quality, organic wine and unfiltered/unpastuerized beer is a part of the heart healthy approach.
Calcification: Why Is Your Calcium Score So High?
Calcification of the arteries occurs when calcium is deposited into the arteries instead of bones and teeth. This occurs from a vitamin K2 deficiency, magnesium deficiency, high oxidized cholesterol intake, and low vitamin D/high calcium intake from the diet, supplements or medication that can disrupt calcium metabolism.
For example, several studies have found that people who take Proton Pump Inhibitors that block stomach acid – like Prilosec – have significantly higher arterial calcifications due to the affects on calcium. They also increase the risk for another heart attack in patients who’ve already had one. PPIs skew nutrient absorption, impede liver function and alter the bacterial balance in the intestines, making the heart more vulnerable to inflammation, arrhythmia and oxygen starvation. Statin drugs have also been found to inhibit the synthesis of vitamin K2.
One dietary example of calcification we might see is with a heavy coffee drinker and a low vitamin K2 intake, common in the American diet. The caffeine in coffee causes leaching of calcium from the bones and without enough K2 and magnesium, it can enter into the arteries. Vitamin K2 comes from butter from grass-fed animals but not grain fed (their digestive system converts k1 rich greens to k2), organ meats like liver, egg yolks and certain cheeses including brie and gouda. All of the foods you have been probably told to avoid for a healthy heart.
So if we look at a French meal of coffee with grass-fed cream, sourdough baguette with brie, pate or foie gras, fresh fruit and pastured eggs cooked in butter, vs. the American version of a double mocha cappuccino with 60 grams of sugar, feedlot pasteurized cream or cream substitute with hydrogenated oils, feedlot egg white omelet cooked in vegetable oil, high glycemic non-fermented bread with feedlot butter or butter substitutes, you see how two versions of the same foods can react completely differently.
One diet is high in omega-3’s, CLA, A, D, E, and K, vitamin C, K2 and b-vitamins, while the other is high in omega-6 fatty acids, sugar, chemicals and oxidized oil while being deficient in K2 and others. One will protect your arteries and keep them clean, and one will cause calcification, inflammation and plaque.
Culinary Techniques to Reduce Toxic Compounds
The way food is prepared and combined plays a major role with potential toxic compounds that have been of concern. For example, when you BBQ, you increase two potentially carcinogenic compounds from the use of high heat. High heat also increases the formation of advanced glycogen end products (AGE’s) from glycation when sugary marinades are used, which is why sugary BBQ sauces should be avoided.
Traditional culinary techniques have addressed ways to minimize toxins. We know that cooking meat in broth instead of high heat is a safer option, and that soups and stews over low heat are going to be the safest way to cook. Second is to cook in saturated fats and use plenty of herbs especially garlic and rosemary. Or use a marinade with olive oil, vinegar, garlic and other herbs, adding vegetables like Brussels sprouts and broccoli, or fermented veggies like sauerkraut or fermented beets, and consuming a small amount of a fermented drink like beer, wine or Kombucha also helps neutralize toxins due to the yeast. By doing this, you eliminate more than 90 percent of the carcinogenic effects, which the remaining can be taken care of by a healthy detoxification system.
What You Need to Know about Your Cholesterol Numbers and Statin Drugs
Let’s talk about your cholesterol levels. The main focus of many doctors today. Your cholesterol levels rise in the winter months and fall during the summer. They go up when you have an infection when you are stressed and during or after a heart attack. You could find a change in score by 20 points without changing anything by multiple tests within a few days, weeks or months.
The current medical guidelines promote the idea that the lower the cholesterol, the better protection you have against heart attacks and strokes. The current aim now for cholesterol levels are less than 180, and even children are being considered for cholesterol-lowering drugs. A recent January issue of American Heart Journal found that 75% of patients hospitalized for a heart attack had “normal” cholesterol levels and close to 50% had LDL levels less than 100 mg/dl.
In the Framingham study that is often cited, four of five people fell into a large middle range of cholesterol levels, whether or not they developed heart disease. Those with extremely low total cholesterol (less than 150 mg/dL) had low (though not zero) risk for heart attack, however those with low cholesterol have an increased risk of dying from gastrointestinal and respiratory diseases. T
hose with extremely high cholesterol (greater than 300 mg/dL) had a higher risk for heart attack (threefold higher). But the great majority of people fell in between these extremes, and the greatest number of heart attacks developed in people with cholesterol levels in this middle range. This is why predicting the risk of heart attacks based total cholesterol, HDL and LDL alone has been called as accurate as flipping a coin.
You may remember Bill Clinton – known for years for southern fried cooking in vegetable oil and sugar – having a greater than 90 percent blockage of all three coronary arteries and going under a quadruple coronary bypass operation in 2004. But in 1993, Dr. Dean Ornish paid a visit to the White House and enlighten the French chefs about cooking low-fat and restricting animal foods. President Clinton took this seriously and banished fat from the White House. Their fat loving French chef couldn’t follow this type of cooking, and was asked to resign.
According to his cardiologist, Bill Clinton did everything right since his 2004 bypass, including a plant based diet, exercising, and keeping his blood pressure and cholesterol in check at 179mg/dl with a statin drug. Despite this, in 2010 Clinton had chest pain, and needed emergency surgery to put two stents into one of his coronary arteries. This lead the associated press to proclaim “there is no cure for heart disease, Clinton’s case shows.” Clinton no longer follows a vegan diet.
The “Good” HDL Cholesterol
The higher the better according to the American Heart Association. HDL is often called the “good cholesterol.” There is conflicting information regarding the importance of the number. It is naturally higher in women than men. In women, estrogen raises HDL and goes down as estrogen does. In men, optimal testosterone lowers it, but makes it more effective at reverse cholesterol transport, which is taking cholesterol back to the liver.
A 2012 study in The Lancet showed that raising HDL levels may not make any difference to heart disease risk, and people who inherit genes that give them naturally higher HDL levels have no less heart disease than those with lower HDL levels. However, another study found that when triglycerides were high and HDL was low, heart attack risk went up 16 times.
The “Bad” LDL Cholesterol
According to the most recent guidelines from the American Heart Association, “Low LDL cholesterol level is considered good for your heart health. However, your LDL number should no longer be the main factor in guiding treatment to prevent heart attack and stroke. For patients taking statins, the guidelines say they no longer need to get LDL cholesterol levels down to a specific target number.
Why would the American Heart Association make this statement? A study from The Lancet show that higher HDL does not necessarily provide more protection, and because studies show “there is no scientific basis to support treating to LDL targets” and “the safety of treating to LDL targets has never been proven.”
This is an important point to understand. When assessing your cardiovascular risk, there are many other factors that should have your attention over getting your LDL below 100mg/dl. Can you have a heart attack if you have low cholesterol? Yes. Can you survive to the age of 95 and never have a heart attack despite high cholesterol? Yes. Can you suffer a debilitating or fatal heart attack with “normal” cholesterol? Yes. Can people who take a cholesterol-lowering medication can still suffer a heart attack? Yes.
What You Should Really Know about LDL
The LDL number as an indicator of heart disease does not hold up against scientific scrutiny, and calling it the “bad cholesterol” isn’t necessarily accurate either. To show a positive correlation, a recent study from Texas A&M University discovered that in a study of 52 adults aged 60-69, those with high levels of LDL developed the most muscle mass after vigorously working out. “People often say, ‘I want to get rid of all my bad (LDL) cholesterol,’ but the fact is, if you did so, you would die,” the Texas A&M professor adds. “Everyone needs a certain amount of both LDL and HDL in their bodies. We need to change this idea of LDL always being the evil thing – we all need it, and we need it to do its job.”
The current theory is that the particle size is the most important aspect of LDL, making large fluffy LDL harmless and small sticky LDL capable of damage and inflammation. Small LDL particles are more prone to oxidation, which stimulates the release of inflammatory and adhesive proteins aka plaque.
Oxidation and glycation (from high blood sugar) are the primary concerns, which transforms LDL from cholesterol transport vehicles into highly reactive molecules capable of damaging the delicate endothelial cells that line our arterial walls and increasing plaque.
Think of LDL like ships in the bloodstream. A healthy ship has CoQ10, beta-carotene, lycopene, lutein, and vitamin E (mainly gamma-tocopherol, vitamin C recycles E) aboard to act like cannons against oxidation. If blood sugar is normal, the ship isn’t affected. But if blood sugar is high, they attach onto the ship, poke holes and make it vulnerable to free radicals that cause oxidation, which are kind of like pirates under the trans-fat and vegetable oil command. High blood sugar and low amounts of these antioxidants make small dense LDL vulnerable to be attacked and oxidized.
A new analysis followed over 1,000 men in their mid-40s to mid-50s for more than 12 years. After adjusting for other stroke risk factors, such as older age and diabetes, they found that men with the highest blood levels of lycopene were 55 percent less likely to have a stroke than those with the lowest. Lycopene is high in tomatoes, but also found in guava, apricots, papaya, watermelon and pink grapefruit.
What happens is your immune systems spots the glycated, oxidized small LDL particles, and sends out macrophages to engulf as many as possible to remove it. But the macrophages get overwhelmed trying to remove them and expand, can’t fit through the exit and become trapped. Cytokines – which are like little grenades – are released by the macrophages in an attempt to get out, damaging the arterial wall, building plaque and disrupting blood flow.
WGA in modern refined wheat products have also been found to stimulate immune cells to release cytokines. It turns out these excessive cytokines are now being explored as a major cause of depression, showcasing the link between heart disease and depression. So it is your immune system’s response to inflammation by clearing the blood of these damaged ships that makes small, dense LDL particles increase the likelihood of developing coronary plaque and suffering a heart attack by 300 percent.
Statin drugs deplete the main antioxidant CoQ10, and therefore increases the risk of LDL oxidation. A poor diet low in vegetables and fruits, nuts and seeds leads to low levels of beta carotene, lycopene and lutein, and vitamin E. Vitamin C and B-vitamins are needed for production of CoQ10, and recycling vitamin E. For back up protection, a unique polyphenol in pomegranates, reseveratrol in wine, and certain compounds in green tea, black tea and the spice turmeric have been found to have the highest activity for also protecting LDL against oxidation.
How to Treat Small Dense LDL
The best way to “treat” small-particle LDL’s is by lowering triglycerides through eliminating refined sugar and excess refined carbs, vegetable oils and trans-fats, exercise and lowering stress, anxiety and depression. There is no drug treatment available that affects LDL particle size, including Statins. High blood sugar and low antioxidants are the main cause of high glycated hemoglobin (A1C) and small LDL particles to become oxidized, leading the cascade of damage to the blood vessels – which is how diabetes quadruples the risk of heart disease. Another reason why a focus on protein and fat – macronutrients that stabilize blood sugar – makes the most sense for a heart healthy diet.
Fish oil helps lower triglycerides and promote a shift from small, dense LDL particles to larger, “fluffier” LDL particles, along with the omega-3 fatty acids known to lower inflammation and reduce cardiovascular risk.
What You Should Be Looking For On Your Blood Work
Lp(a) <14mg/dl: Lp(a) is a substance that is made up of an LDL part plus a protein (apoprotein a). It is a sticky form of LDL. Elevated Lp(a) levels are a very strong risk factor for heart disease, if not one of the highest. Lp(a) not only is a direct cause of plaque growth and the plaque rupture that can cause a heart attack, but it also magnifies the dangers of all other risk factors, especially LDL particle size.
While it is believed to be genetic and difficult to lower, Linus Pauling theorized that Lp(a) serves as a surrogate for vitamin C due to a gene mutation that occurred when we lost the ability to manufacture vitamin C millions of years ago. His hypothesis was when vitamin C is too low, it can cause Lp(a) to elevate.
One study found that the milk protein casein decreased Lp(a) by 50 percent, but soy increased it by 20 percent. Consider the major increase in soy oil and this connection to heart disease. Another found that optimal testosterone levels in men and estrogen levels in women can lower Lp(a) by 25%. L-carnitine has also been found to possibly lower Lp(a), with the highest amount found in red meat.
Homocysteine: Homocysteine is a normal by-product of protein digestion, but in elevated amounts it causes cholesterol to be oxidized (free radical damage, platelets sticking together, and can attack blood vessel walls). If you lack certain protein enzymes, b-vitamins, magnesium or have hypothyroidism, homocysteine can rise. T
he American Heart Association downplays the significance of high homocysteine, even though their website shows it is related to heart disease and that b-vitamins lower it (magnesium should be included as well because the major enzymes in homocysteine metabolism require magnesium).
Researchers have concluded that homocysteine is up to forty times more predictive than cholesterol for assessing risk of cardiovascular disease. 32% more heart attack patients had homocysteine levels above 10 µmol/L. 500% more heart attack patients had homocysteine levels above 15 µmol/L.
Two things stand out to me about homocysteine. The first is that if a high protein diet can cause it, is this rise due to the focus on lean meats instead of organ meats, the later of which have ample supplies of b-vitamins while lean meats have less? The second is the rising prevalence of the gene mutation MTHFR, which disables peoples ability to absorb folate and B12 unless they are in the methylated form.
Triglycerides <150: While triglycerides by themselves do not cause heart attacks, they are the driving force behind lipoprotein particles that are potent causes of heart disease, such as small LDL and very low-density lipoprotein (VLDL). In general, aim for a triglyceride level below 100 mg/dL, as all triglyceride-rich particles (including small LDL) are minimized at this level. Lowering your sugar (even sugary fruit) and refined grain intake, lowering body fat, exercise and increasing healthy fat are all effective strategies. Fish oil and vitamin C are both effective ways to lower triglycerides and VLDL by 30–50%.
C-Reactive Protein: The American Heart Association downplays its significance. C-Reactive protein is a measure of inflammation and a strong indicator of blood vessel damage. In one study, the men who had the highest levels of C-reactive protein were more than twice as likely to suffer from heart disease. Elevated C-Reactive protein shows a heart attack risk by almost 600% when above 3.00mg/liter. Low testosterone and high in estrogen in men, lack of probiotics, obesity, sugar, stress, refined vegetable oils and high-glycemic carbohydrates increase C-reactive protein.
Hypothyroidism is also associated with an increase in C-reactive protein level. In one study of non-diseased, overweight non-smokers who received 1000mg of vitamin C and started out with elevated C-reactive protein levels > 1.0 had 25% lower CRP levels compared with the placebo group after only two months, likely due to its protective effect against oxidation and cytokines. The researchers concluded that “vitamin C’s magnitude of the effect was similar to Statin’s,” – but without the side effects – and should be investigated for its role in reducing chronic inflammation.
Calcium Score <100: Calcification occurs from a vitamin K2 and magnesium deficiency, both which direct calcium into the bones instead of the arteries. Very high vitamin D levels can also cause calcification. It can also occur from medications like proton pump inhibitors.
Vitamin K2 is found in butter, egg yolks, liver, natto, gouda and brie cheese. Magnesium is best supplemented as magnesium citrate or citramate, since our water and top soil has become severely depleted.
TSH, T3 and T4. Thyroid hormone also has direct anti-atherosclerotic effects such as blood vessel dilatation. Carnivores are free of atherosclerosis with their standard fare of saturated fat and cholesterol until you take out the thyroid gland. Then they get blood vessel damage just like herbivores.
Hypothyroidism has become something of a silent epidemic. The thyroid hormone is the central governor of the LDL receptor, and the LDL receptor is the central governor of clearance of LDL cholesterol from the blood. So, the thyroid hormones basically communicate to our cells to take the LDL cholesterol from the blood and make DHEA, testosterone, estrogen and progesterone.
For your diet, iodine, selenium, magnesium (evidence supports hypothyroidism being a magnesium deficiency) and riboflavin intake along with filtering fluoride and chlorine from your water, and avoiding mercury from large fish, pesticides and bromides in certain sports drinks, sodas and bread help normalize the thyroid. Statins inhibit the biosynthesis of selenium-containing proteins such as glutathione peroxidase that suppresses peroxidative stress.
Blood Pressure 120/80. Reducing your systolic blood pressure by 20 millimeters (regardless of how high your blood pressure currently is) decreases your risk of stroke by 50 percent. Reduce it by another 20 mm, and you cut your individual risk in half yet again. Not smoking, or quitting smoking equated to a 40 percent lower risk.
Sugar, obesity, high coffee intake, inactivity, and stress will spike blood pressure. Low magnesium, low potassium levels and low vitamin D levels combined with a high sodium content will increase blood pressure. A recent study showed that increasing potassium-rich foods to 4.7 grams was equivalent to cutting out 4 grams of sodium in terms of reducing blood pressure.
Weight loss, cutting out sugar and excess carbs, exercise, stress relieving activities, pets, meditation, Qi Gong, magnesium, vitamin C, E, carotenoids and CoQ10 all regulate blood pressure.
Iron: Iron can cause oxidation of cholesterol, so if you have excess iron levels you can damage your blood vessels and increase your risk of heart disease. Checking your iron levels is advised. Men should not take iron supplements.
HbA1C 4.0-5.9: When blood glucose levels are high, glucose molecules attach to the hemoglobin in red blood cells. Normal levels of glucose produce a normal amount of glycated hemoglobin. Too much causes oxidized LDL leading to plaque, stiffening of the collagen in the blood vessel walls and leading to high blood pressure, especially in diabetes.
High levels also cause weakening of the collagen in the blood vessel walls, leading to strokes. Vitamin C and Vitamin E may lower HbA1C levels by reducing the rate of glycation of hemoglobin. A deficiency of B12 and iron may also lead to higher HbA1C levels, as well as chronic use of NSAID’s (Aspirin, Tylenol etc). Other medications should also be explored if high levels are unexplained.
What Statin’s Deplete
Statin drugs work by inhibiting the enzyme HMG reductase, which is needed for the production of cholesterol. The problem is that this enzyme leads to A LOT more than just cholesterol.
1. Lower’s Testosterone and DHEA: Just like a low-fat, high fiber diet, Statin drugs have been found to lower testosterone. I have written about low testosterone levels showing up in younger men with each generation and the ramifications of that in this article.
I believe it is becoming extremely prevalent, but a lot of guys don’t get tested for it so they don’t realize it is low. Men whose testosterone levels were slightly above average were 45% less likely to have high blood pressure, 72% less likely to have experienced a heart attack and 75% less likely to be obese than men whose levels were slightly below average.
2. Depletes CoQ10: At age 20, CoQ10 is higher in the heart than any other organ. By age 80, the levels are cut in half. This is arguably the most important nutrient for the heart, and statins reduce this amount of CoQ10 dramatically lower. Low CoQ10 levels are found in those with heart disease.
CoQ10 has been shown to protect against stroke, benefit cardiovascular disease, promote younger skin, prevent migraines, improve glucose control, fight cancer, and improve high blood pressure. It is also the most important nutrient for the gums, which is why low CoQ10 causes poor gum health, and poor gum health is connected to heart attack risk. Beta Blockers also deplete CoQ10, as do other types of antihypertensives and vasodilators.
3. Depletes Squalene: Squalene is a major antioxidant produced by the body to combat inflammation in the skin and eyes, aids in detoxification and has anti-cancer activity. This depletion could be why Stains increase the risk of cataracts and cancer (along with CoQ10). Olive oil is a good source of dietary squalene.
4. Depletes A, D, E, K2, B12, Folate, Zinc and Phosphate: The vitamins A, D, E, K2, folate, calcium and magnesium are all crucial for a healthy functioning heart.
5. Increases Blood Sugar: A study published in the Archives of Internal Medicine found a nearly 50 percent increase in diabetes among longtime statin users. A 2011 analysis in the Journal of the American Medical Association and a 2010 analysis in The Lancet also found a higher risk of diabetes among those taking cholesterol-lowering drugs.
This is because cholesterol is the precursor to glucocorticoids, which regulate blood sugar levels, and mineralocorticoids, which regulate mineral balance. According to the American Heart Association, Adults with diabetes are two to four times more likely to have heart disease or a stroke than adults without diabetes. High blood sugar is also connected to Alzheimers and Dementia, being referred to as Type 3 diabetes. Another study found that that high spikes in blood sugar was enough to drop testosterone levels by as much as 25% in a random grouping of healthy, prediabetic, and diabetic men.
Side Effects of Statin Drugs
How about the side effects that the patients are often unaware of the cause? The side effects include heart failure, neuropathy, cancer, elevated liver enzymes, muscle pain (can lead to muscle damage and rhabdomyolysis), dizziness, suppressing of the immune system, joint pain, weakness, headache, rash, nausea, heartburn, constipation, diarrhea, gas, memory loss, urinary tract infection and depression (people with depression are up to 40 percent more likely to die from heart disease than people without depression).
So what we are really seeing are the side effects of low cholesterol, low CoQ10 status, deficient levels of vitamins and minerals and poor hormone production. Muscle pains and memory problems are by far the most common side effects I see, and a connection to dementia wouldn’t be a far off hypothesis.
Why Are Statins Promoted if All of this Known?
So you are probably wondering with this knowledge in hand, why Statins are recommended in the first place. The simple answer is that many doctors are still convinced that high cholesterol is the most important risk factor for preventing heart disease and will cite studies in favor of Statins. But here is the truth about those studies:
#1 The big five that are usually cited found that risk of non-fatal heart attack and stroke were reduced by 1.4% in people on statin drugs – but the rate of death or serious hospitalization went up 1.8%. 1 Not the best trade off.
#2 There is no relationship between blood cholesterol and heart disease risk in women over fifty or men over seventy. In fact, for older people, deaths were more common with low cholesterol and those who lived the longest had high cholesterol. According to the authors of the recent 2015 study in Expert Review of Clinical Pharmacology, “Our opinion is that although statins are effective at reducing cholesterol levels, they have failed to substantially improve cardiovascular outcomes.”
#3 Statins have been shown to help with heart attacks and stroke in those that have suffered a heart attack or stroke, or possibly those with hypercholesterolemia (mid 300’s). For some people, the reason for having cholesterol levels that high isn’t clear, but looking at TSH, T3 and T4 of the thyroid is a good start. For this subgroup, the best approach is to supplement your prescription if you choose to use Statins.
DIET SUMMARY

Sources
1. Supplement Your Prescription: What Your Doctor Doesn’t Know About Nutrition by Dr. Hyla Cass, MD.
2. Khaw KT, Bingham S, Welch A, et al. Relation between plasma ascorbic acid and mortality in men and women in EPIC-Norfolk prospective study: a prospective population study. European Prospective Investigation into Cancer and Nutrition. Lancet. 2001 Mar 3;357(9257):657-63.
3. Yokoyama T, Date C, Kokubo Y, Yoshiike N, Matsumura Y, Tanaka H. Serum vitamin C concentration was inversely associated with subsequent 20-year incidence of stroke in a Japanese rural community. The Shibata study. Stroke. 2000 Oct;31(10):2287-94.
4. Brown DJ, Goodman J. A review of vitamins A, C, and E and their relationship to cardiovascular disease. Clin Excell Nurse Pract. 1998 Jan;2(1):10-22.
5..Myint PK, Luben RN, Welch AA, Bingham SA, Wareham NJ, Khaw KT. Plasma vitamin C concentrations predict risk of incident stroke over 10 y in 20 649 participants of the European Prospective Investigation into Cancer Norfolk prospective population study. Am J Clin Nutr. 2008 Jan;87(1):64-9.
6. Ye Z, Song H. Antioxidant vitamins intake and the risk of coronary heart disease: meta-analysis of cohort studies. Eur J Cardiovasc Prev Rehabil. 2008 Feb;15(1):26-34.
7. Myint PK, Luben RN, Wareham NJ, Bingham SA, Khaw KT. Combined effect of health behaviours and risk of first ever stroke in 20,040 men and women over 11 years’ follow-up in Norfolk cohort of European Prospective Investigation of Cancer (EPIC Norfolk): prospective population study. BMJ. 2009;338:b349.
8. Pfister R, Sharp SJ, Luben R, Wareham NJ, Khaw KT. Plasma vitamin C predicts incident heart failure in men and women in European Prospective Investigation into Cancer and Nutrition-Norfolk prospective study. Am Heart J. 2011 Aug;162(2):246-53.
9. Yildiran H, Mercanligil SM, Besler HT, Tokgozoglu L, Kepez A. Serum antioxidant vitamin levels in patients with coronary heart disease. Int J Vitam Nutr Res. 2011 Jul;81(4):211-7.
10. Aviram M, Rosenblat M, Gaitini D, et al. Pomegranate juice consumption for 3 years by patients with carotid artery stenosis reduces common carotid intima-media thickness, blood pressure and LDL oxidation. Clin Nutr. 2004 Jun;23(3):423-33.
11. Primal Panacea by Levy, Thomas E, MD, JD.







Thank you for this fascinating, in-depth article. It is the clearest, most well researched article on heart disease and stroke I have seen. I finally feel like I understand this complex health issue and now have the tools to prevent it. It is refreshing to see an article on this subject that cuts through the mainstream, incorrect information being forced upon the public and actually tells us the truth.
Alex: This is a masterful piece of writing!! So well written and organized! Thank you for sharing your research and the results of your efforts in such a thoughtful and reflective piece and on your Website.
Hi Judith,
Thank you very much! I think this was probably my favorite research topic so far, and I hope that it sparks a dialogue towards the right answers for preventing these diseases.
Hi Erin,
Thank you for the feedback. I am so glad you found it informative!
This is an extremely interesting article, filled with great information. I hope you will continue
to get this message out not only to the believers like myself but to the masses, who are in such need
of nutritional guidance. Keep up the good work!
Thank you so much Valerie!
Hello Alex- In the above article you state:
“Homocysteine is a normal by-product of protein digestion, but in elevated amounts it causes cholesterol to be oxidized…”. Will protein supplements(whey) increase homocysteine levels?
Great article, many thanks!
Hi Matt,
As long as your folate, B6, B12 and choline intake is matching your protein intake, homocysteine should stay in range with the addition of whey protein.