The American Heart Association will have you believe that the biggest dietary concern is “reducing sodium and increasing whole grains.” If you have followed any nutrition research over the years, you will see that there is much more to the dietary picture than that. And if you are privy to how the lobbying industry works, you will know why sugar and vegetable oils are not called out. Ever since I gave a lecture on the dietary connection to heart disease and posted it online, I have attempted to simplify the dietary information to reach more people.
I think one of the best ways to help reduce the risk of cardiovascular disease is to know what to focus on with your blood work. If you have cardiovascular disease in your family, I highly recommend doing a Nutrition Genome Report so that you have genetic information and blood work for the most accurate program.
How to Read Your Cardiovascular Bloodwork in 5 Easy Steps
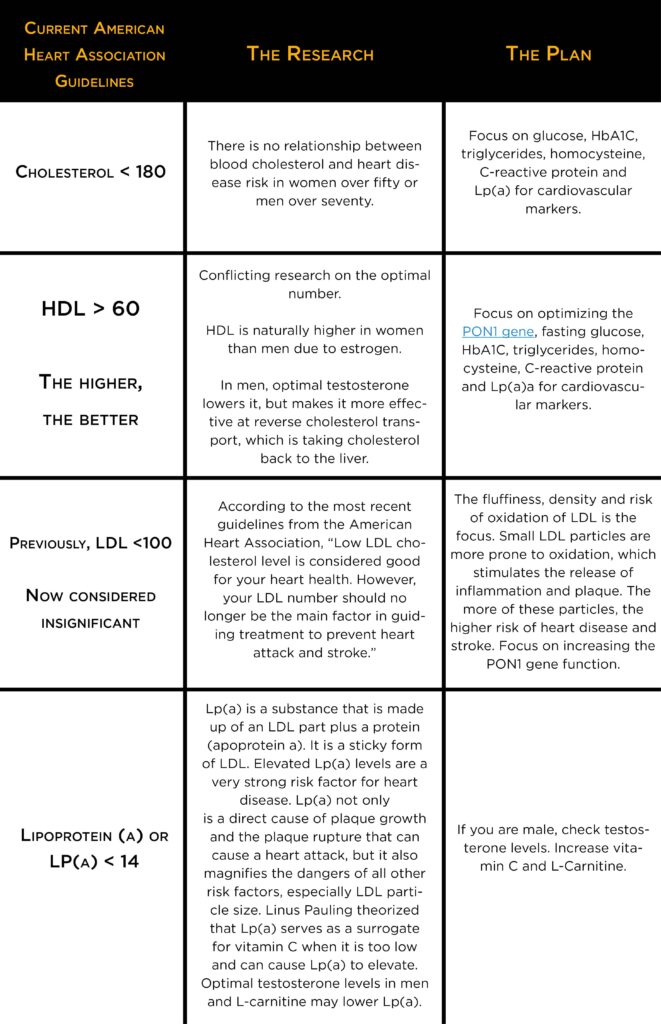
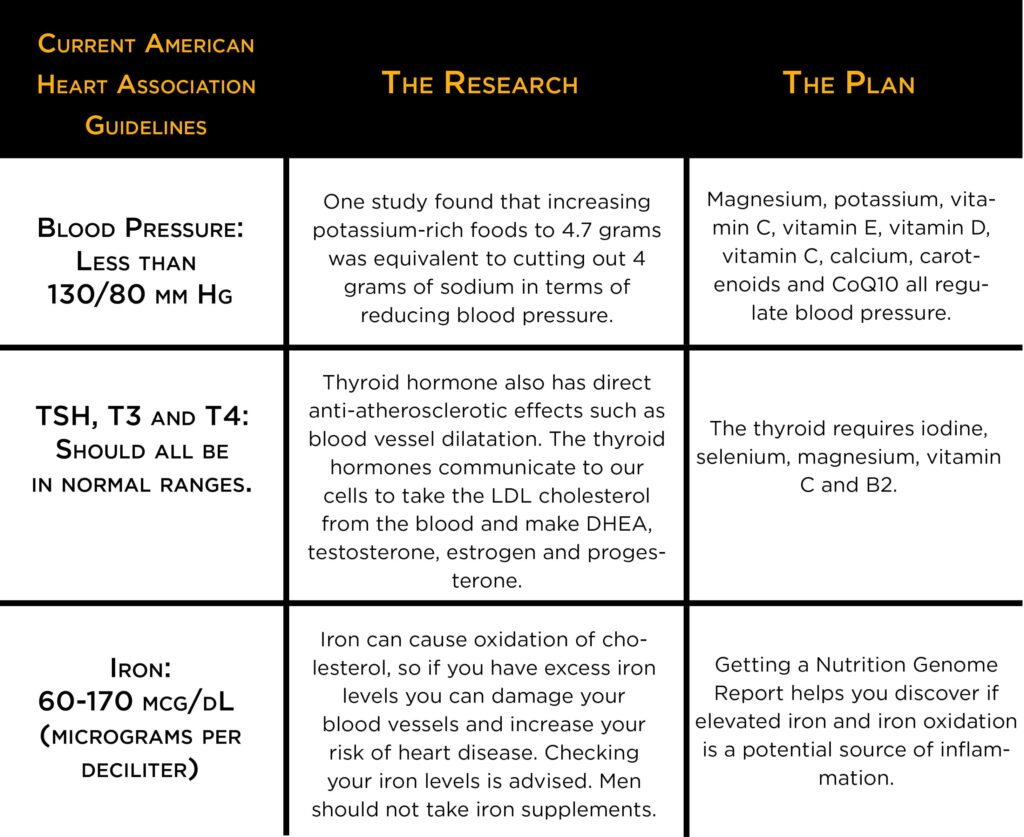
I have put together multiple quick reference tables for you to organize and decipher your blood work for cardiovascular health. As you will see, I have outlined what the American Heart Associated has outlined and is used in most doctors offices. To the right, you will see what the actual research has found and what to do about it.
If you do not see any of these on your routine blood work, request them. Homocysteine is a common one that isn’t tested. Whether you are male or female, in your 30’s, 60’s or 90’s, it is relevant for everyone.
1. Cholesterol
HDL is often called the “good cholesterol” and transports cholesterol to the liver and other organs. In women, estrogen raises HDL and goes down as estrogen does. In men, optimal testosterone lowers it but makes it more effective at reverse cholesterol transport, which is taking cholesterol back to the liver. While HDL alone may not directly tell you your risk, one study found that the risk of heart attack went up 16 times for those with the highest triglycerides and lowest HDL.
For patients taking statins, the guidelines say they no longer need to get LDL cholesterol levels down to a specific target number. This is a strange claim because cholesterol-lowering is mainly targeting LDL since doctors try to increase HDL. An issue of the American Heart Journal found that 50% of patients hospitalized for a heart attack had LDL levels less than 100 mg/dl. Now if your triglycerides are in the normal range, you are not targeting the LDL number and trying to raise HDL, what does this tell you about the alleged importance of lowering total cholesterol?
Now, what if cholesterol is very high, say in the mid 300’s or more? Look at your thyroid panel. The thyroid hormone is the central conductor of the LDL receptor, and the LDL receptor is the central conductor of the clearance of LDL cholesterol from the blood. Hypothyroidism could be the cause. The thyroid gland requires magnesium, vitamin C, zinc, iodine, selenium, and B2.
Make sure your thyroid is in order and have a glass of organic wine (or wine from Italy or Argentina) with your healthy dinner to increase HDL and protect LDL from oxidizing, which is the real concern with LDL. Alcohol in small amounts – 5 oz. of wine daily for example – makes the gene PON1 work 395% better to protect against LDL oxidation, but over that amount leads to a 45% decrease in function. Learn more about optimizing PON1 here.
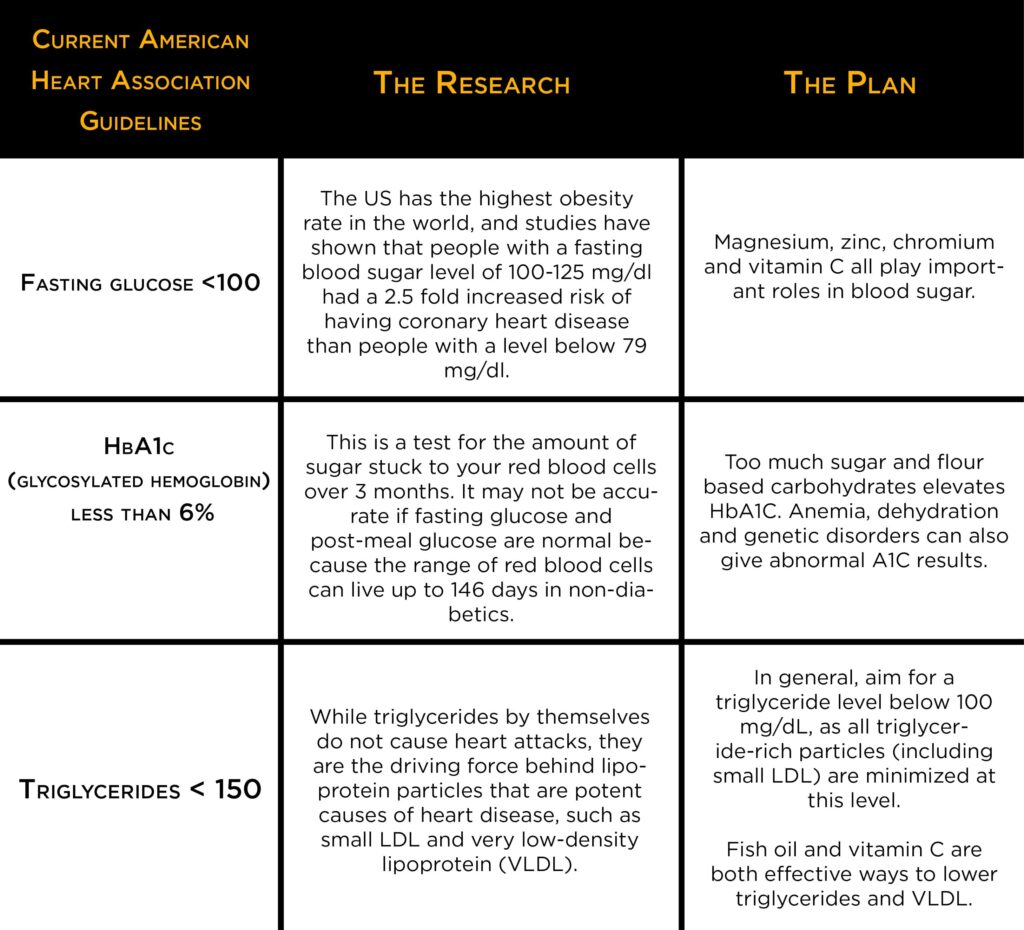
2. Blood Sugar
Fasting Glucose and A1C: When blood glucose levels are high, glucose molecules attach to the hemoglobin in red blood cells. Normal levels of glucose produce a normal amount of glycated hemoglobin. Too much causes stiffening of the collagen in the blood vessel walls, leading to high blood pressure, especially in diabetes. High levels also cause weakening of the collagen in the blood vessel walls, leading to strokes. A deficiency of B12 and iron may also lead to higher HbA1C levels, as well as the chronic use of NSAID’s (Aspirin, Advil). Other medications should also be explored if high levels are unexplained.
Triglycerides: Triglycerides can easily be kept in range with a good diet low in sugar and flour-based foods while supplementing with vitamin C and fish oil.
See my vitamin C recommendations here.
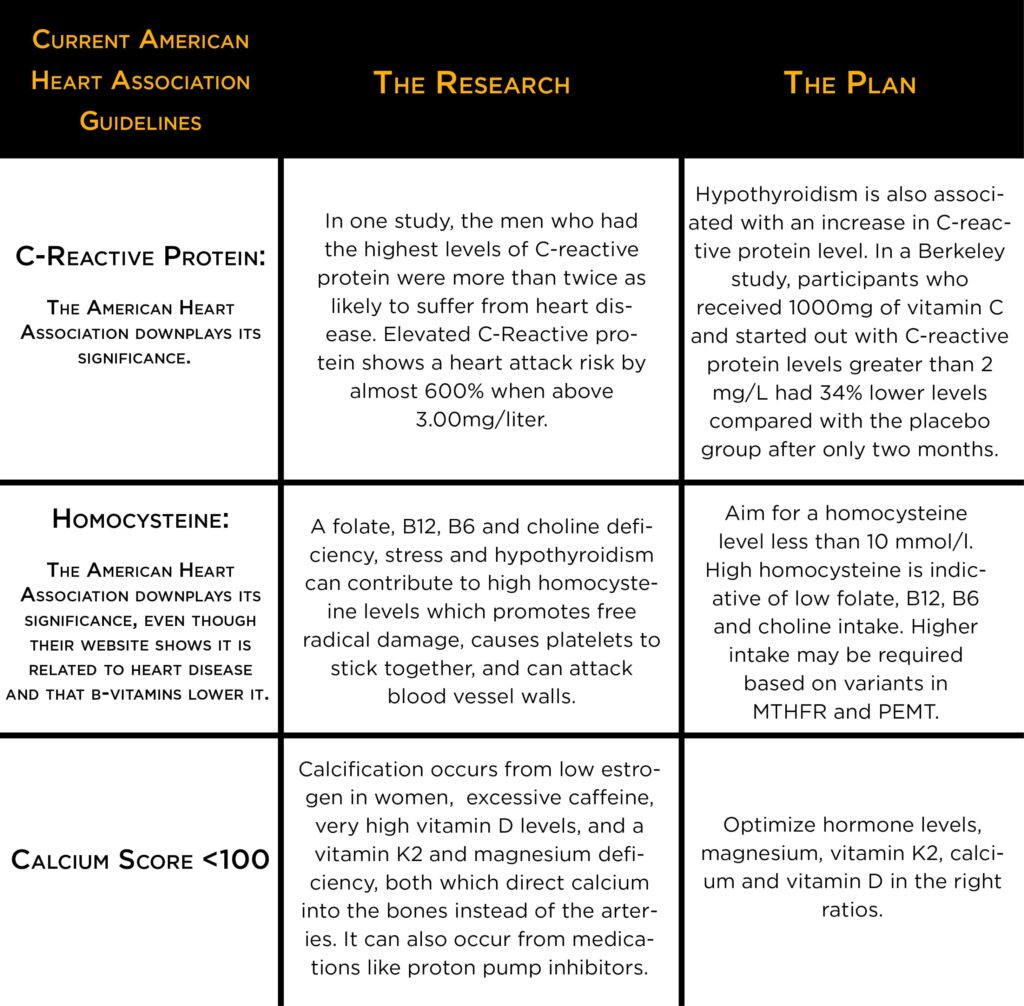
3. Inflammation
C-Reactive Protein: A measure of inflammation and a strong indicator of blood vessel damage. Hypothyroidism, low testosterone and high in estrogen in men, sugar, refined vegetable oils, high-glycemic carbohydrates, low vitamin C, excessive exercise and stress increase C-reactive protein. One study reported that three weeks of beer consumption significantly reduced the level of plasma c-reactive protein (CRP), but was attributed to the alcohol.
Homocysteine: A folate, B12, B6 and choline deficiency, stress and hypothyroidism can contribute to high homocysteine levels and free radical damage, causes platelets to stick together and can attack the walls of the blood vessels.
Researchers found that the normal higher limit of homocysteinemia levels should be reduced, as the values found in this over 14 µmol/l, were associated with a risk of 2.03 for coronary disease. Another study found that approximately 30% of a group with coronary heart disease had homocysteine levels above 15 mmol/l.
High homocysteine is indicative of a b-vitamin deficiency of folate, B6, and B12, and may be connected to the MTHFR, CBS and PEMT gene variants that require higher doses of folate, B6, B12, and choline.
See my B-vitamin recommendations here.
4. Blood Pressure, Thyroid and Iron Levels
Blood pressure goes up with too much sugar in the diet, excess weight, stress, low testosterone, low magnesium, potassium, vitamin C, vitamin D, vitamin E, carotenoids, and CoQ10. See how to get enough magnesium, potassium, vitamin E and other nutrients in your diet here. Check your vitamin D levels on your blood work and check your testosterone.
Men whose testosterone levels were slightly above average were 45% less likely to have high blood pressure, 72% less likely to have experienced a heart attack and 75% less likely to be obese than men whose levels were slightly below average. The optimal level appears to in the 550-900 ng/dl range to reduce risk according to the American College of Cardiology. See how to raise your testosterone levels naturally here.
The thyroid gland requires selenium, iodine, vitamin C, zinc, magnesium, and B2 (riboflavin). See how to get these nutrients here.
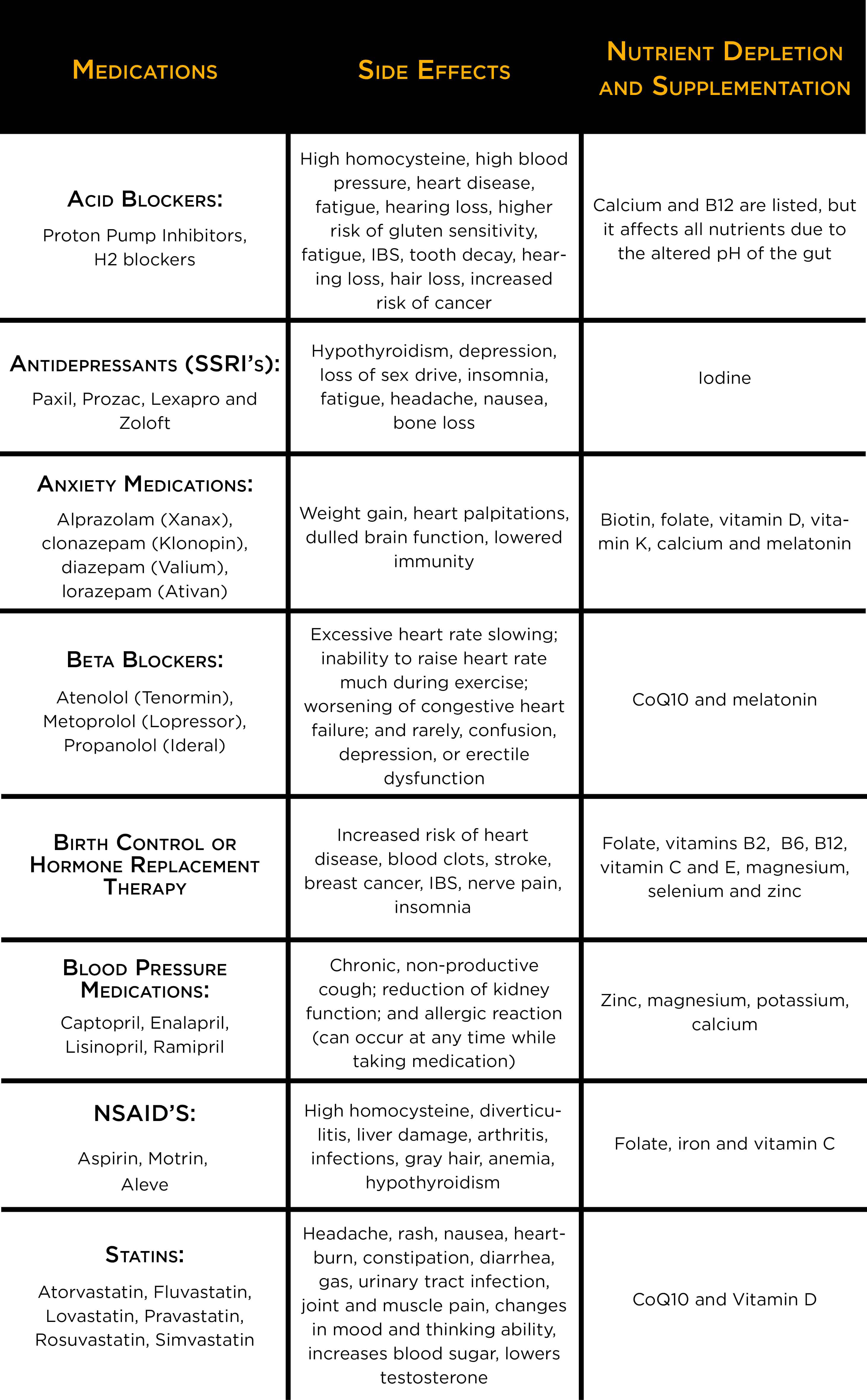
5. Check Your Medications!
You would be surprised to see how often it is the medications that are causing health issues in the first place. After all, prescription drugs are the 4th leading cause of death, tied with strokes.
You may not be told of the side effects or nutrient depletions caused by your medications and it is up to you to do your homework. Here is a chart for your convenience of commonly used medications.
Other Sources for Studies
- Supplement Your Prescription by Hyla Cass MD
- Drug Muggers: Which Medications Are Robbing Your Body of Essential Nutrients – and Natural Ways to Restore Them







Thank you. i am very grateful for your article.
fiona
Thanks for the comment Fiona. It is very appreciated.
Trying to gather which blood tests are ideal to have checked as part of a general physical… glucose, HbA1C, triglycerides, homocysteine, c-reactive protein, and Lp(a). Would you also suggest having TSH, T3, T4 and iron tested as well? It seems based on your article that you don’t find cholesterol, HDL, nor LDL to be worthwhile, is that correct?
Hi Nicole,
I would absolutely look at TSH, T3, T4, and iron. Based on the evidence, looking at just the HDL and LDL number to determine your current cardiovascular risk is not accurate. The VAP test gives you a better idea of LDL particle number and particle size, which is more relevant. This article goes more in-depth on cholesterol, HDL and LDL: http://paleoedge.com/the-diet-myths-about-heart-disease-strokes/
Hey Alex, if I go with Thorne Basic Nutrients 2aday, for my d & k and b’s, do I need the whole food b’s by Pranin? Thanks George
Hi George,
No, you wouldn’t need the whole food B’s by Pranin if you are taking the Thorne Basic Nutrients.
You have Tylenol listed as an NSAID however it isn’t. Is that in error or is there a specific reason why it was included?
Hi Michael,
Thank you for pointing that out. That should have said Advil, not Tylenol. Fixed.
Thanks for this, I’ve learn a lot.
Hi Robert,
No problem! Thank you for commenting.